Antibiotics and Probiotics- Why you shouldn't take either without a good reason
As most people know, antibiotics are used to kill bacteria in our bodies. Recently products known as probiotics have become popular. For those who don't know what they are, probiotics are meant to promote the growth of bacteria in our body, primarily in our gut. In theory antibiotics are used to kill harmful bacteria and probiotics are meant to promote the growth of good bacteria but is anything ever that simple? We are starting to learn that the answer to that question is a resounding no.
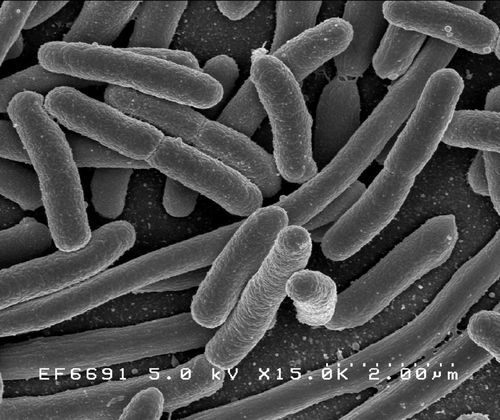
One of the problems with this idea is that our understanding of bacteria has been a bit naive. The microscopic world of living things isn't really made up of good bacteria and bad bacteria any more than the human world is made up of good people and bad people. Some bacteria may be mostly good, others mostly bad, with the majority being somewhere in the middle, but every bacteria may have characteristics that may make it good or bad depending on the situation and the company it keeps just like people.
A Little Background
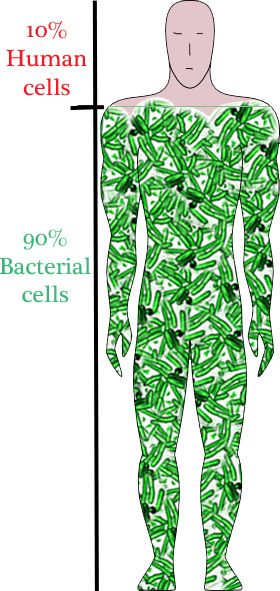
Its been known for a long time that an astounding 90% of the cells in and on our bodies don't belong to us at all. Most of what we consider "us" is really bacterial cells. Our own cells only make up a small percentage of the total. We call this collection of bacteria living in and on our body the Microbiome which is often shortened to the biome. A recent project called the Human Biome Project used new genetic tools to examine these major cohabitants of our bodies in a way that was never possible before. The results were surprising. What they found was that each of our bodies is inhabited by at least a 1,000 different species of bacteria and possibly many more. They also discovered that the type and amount of bacteria each person carries are so specific that a given person's microbiome might be as unique as a set of fingerprints.
Along with the publication of the Human Biome data there has been a lot of research into the effects that our microbiomes have on our health. There is preliminary evidence that certain combinations of bacteria may be associated with a greater or lower risk of diseases such as Diabetes, Obesity, Inflammatory Bowel Disease, and even Alzheimer's as well as many other conditions. They have also found that the biomes of people living in modern societies are less diverse than those of people living in more primitive conditions. This means that those of us in the industrialized world have fewer species of bacteria living with us than people living in the amazon jungle. While there are many theories about why this is so including exposure to antibiotics, no one knows for sure what has lead to the loss of bacterial diversity among people who live in modern societies. What that means for our health we don't know at this point. This research is all in its earliest stages. We have no idea what bacteria are important, how greater or lesser diversity affects health, whether we can make meaningful changes in the bacteria that live among us, or even if those changes would be helpful or harmful.
Along with the publication of the Human Biome data there has been a lot of research into the effects that our microbiomes have on our health. There is preliminary evidence that certain combinations of bacteria may be associated with a greater or lower risk of diseases such as Diabetes, Obesity, Inflammatory Bowel Disease, and even Alzheimer's as well as many other conditions. They have also found that the biomes of people living in modern societies are less diverse than those of people living in more primitive conditions. This means that those of us in the industrialized world have fewer species of bacteria living with us than people living in the amazon jungle. While there are many theories about why this is so including exposure to antibiotics, no one knows for sure what has lead to the loss of bacterial diversity among people who live in modern societies. What that means for our health we don't know at this point. This research is all in its earliest stages. We have no idea what bacteria are important, how greater or lesser diversity affects health, whether we can make meaningful changes in the bacteria that live among us, or even if those changes would be helpful or harmful.
So what does this tell us about the use of antibiotics and probiotics? It means that for all of the reasons mentioned above we need to tread carefully when we take antibiotics that may reduce the number of bacterial species in our biome or take probiotics whose effects we really know very little about despite the varied and growing claims of marketers. Anyone who says they understand the microbiome and that they know how to change it to improve your health isn't telling the truth. We just aren't there yet and when you don't fully understand something its generally best to make as few changes as possible unless its done as part of a research study.
Antibiotics
Antibiotics are one of the most important advances in modern medicine, but just as bacteria are not all good or all bad neither are antibiotics. These drugs are invaluable when we need to treat a dangerous bacterial infection. Over the decades since they were invented antibiotics have saved millions of lives. Initially these drugs were used primarily for serious life threatening infections but as the costs came down and they became widely available antibiotics became victims of their own success. Today many people think of antibiotics as a cure all for more minor illnesses and in many cases they are used for conditions where they are not effective at all.
Bronchitis, sore throats, ear infections, and sinus infections are some of the most common conditions for which antibiotics are prescribed today yet 90% of these conditions are caused by non-bacterial conditions like viruses and allergies which will not respond to antibiotics. Even worse, tens of thousands of people with colds are treated with antibiotics in the US alone every year and antibiotics are completely ineffective in treating these viral infections.
When we use antibiotics for conditions that don't require them two things can happen which are harmful to us. First, antibiotics are indiscriminate. They kill many different types of bacteria including many of the ones which may be performing important functions in the body. When these innocent bystanders are killed there can be short term side effects such as severe diarrhea, or yeast infections, but there may be other long term side effects we don't even know about yet like increased rates of diabetes, cancer, or heart disease. Secondly, bacteria develop resistance to antibiotics when they are exposed to them frequently. Every time you take antibiotics you kill off bacteria which are not resistant and leave behind resistant bacteria to reproduce and increase in number. Each round of antibiotics increases the percent of bacteria that contain resistance genes, and bacteria are voracious collectors and traders of resistance genes. When one bacteria develops resistance the gene can then be passed on to other bacteria. They can even be passed on to bacteria of other species. The use of antibiotics when they are not needed can therefor result in the emergence of a resistance gene which will linger in our microbiome and potentially be passed on to a dangerous organism that invades our body weeks or months later.
This doesn't mean we should never use antibiotics. They are crucial and important drugs when used correctly. The key is to use them correctly. Physicians often prescribe antibiotics because they are short on time and find it far more time consuming to explain to a patient why they don't need antibiotics than it is to just write a prescription, especially if the patient is going to leave angry when they don't get what they want.
When patients feel sick and go to the doctor they should remind the doctor that they have come for a diagnosis, not a specific treatment. Do not tell the doctor that you have been sick too long and want an antibiotic. Don't tell the doctor that you "can't afford to be sick". Nothing will bring out the prescription pad quicker than these sorts of comments. Tell the doctor you will take an antibiotic if you really need one, but you would prefer not to if they think the problem will clear up on its own with rest and time. Most physicians are relieved to know they are dealing with a patient who isn't going to pressure them for antibiotics and will be happy to discuss other options especially if the antibiotic is unlikely to help.
Bronchitis, sore throats, ear infections, and sinus infections are some of the most common conditions for which antibiotics are prescribed today yet 90% of these conditions are caused by non-bacterial conditions like viruses and allergies which will not respond to antibiotics. Even worse, tens of thousands of people with colds are treated with antibiotics in the US alone every year and antibiotics are completely ineffective in treating these viral infections.
When we use antibiotics for conditions that don't require them two things can happen which are harmful to us. First, antibiotics are indiscriminate. They kill many different types of bacteria including many of the ones which may be performing important functions in the body. When these innocent bystanders are killed there can be short term side effects such as severe diarrhea, or yeast infections, but there may be other long term side effects we don't even know about yet like increased rates of diabetes, cancer, or heart disease. Secondly, bacteria develop resistance to antibiotics when they are exposed to them frequently. Every time you take antibiotics you kill off bacteria which are not resistant and leave behind resistant bacteria to reproduce and increase in number. Each round of antibiotics increases the percent of bacteria that contain resistance genes, and bacteria are voracious collectors and traders of resistance genes. When one bacteria develops resistance the gene can then be passed on to other bacteria. They can even be passed on to bacteria of other species. The use of antibiotics when they are not needed can therefor result in the emergence of a resistance gene which will linger in our microbiome and potentially be passed on to a dangerous organism that invades our body weeks or months later.
This doesn't mean we should never use antibiotics. They are crucial and important drugs when used correctly. The key is to use them correctly. Physicians often prescribe antibiotics because they are short on time and find it far more time consuming to explain to a patient why they don't need antibiotics than it is to just write a prescription, especially if the patient is going to leave angry when they don't get what they want.
When patients feel sick and go to the doctor they should remind the doctor that they have come for a diagnosis, not a specific treatment. Do not tell the doctor that you have been sick too long and want an antibiotic. Don't tell the doctor that you "can't afford to be sick". Nothing will bring out the prescription pad quicker than these sorts of comments. Tell the doctor you will take an antibiotic if you really need one, but you would prefer not to if they think the problem will clear up on its own with rest and time. Most physicians are relieved to know they are dealing with a patient who isn't going to pressure them for antibiotics and will be happy to discuss other options especially if the antibiotic is unlikely to help.
Probiotics
The bottom line is that all of this research is extremely interesting and promising but its early days. Selling products such as probiotics and prebiotics at this point is putting the marketing way ahead of the science. Many companies are selling capsules of probiotics and others are putting it in foods like yogurt. Unfortunately most of the claims being made are either exaggerated or have no science behind them at all.
The idea behind probiotics is to take so called "good" bacteria and consume them in such a way as to populate the bowel with them creating a healthier state. There are a number of flaws in this theory based on our current state of knowledge though.
1) We don't know which bacteria are "good" - Some bacteria may be good in certain places and not others or when present in combination with certain bacteria but not others. Remember too that we all have very unique microbiomes and it may turn out that a bacteria which is beneficial in one person may have no effect or even be harmful in someone else.
2) We don't know if we can effectively seed the body with new bacteria - It might seem logical that taking a pill filled with a particular bacteria would allow it to grow inside your bowel like seeding your front lawn but that may not work. The desirable bacteria may be absent because the conditions required for them to grow don't exist in the particular body we are trying to put them in. If you spread seed on a bare dry hard patch of your yard it may remain bare for the same reason it was that way in the first place, not enough water, too little sun or some other condition that wasn't conducive to growth. The same may be true when we try to seed an inhospitable bowel with new bacteria.
3) The microbiome is much more complicated then we thought - A defective microbiome may be missing a lot more than one or two species of bacteria. Trying to seed your bowel with "good" bacteria after they have been presumably wiped out may be like trying to repopulate the rain forest after its been stripped bare by seeding it with a few parrots and rubber trees. You may have a some trees and birds but you wont have a rain forest. Putting probiotics into our guts after our diets or medications have altered the normal collection of species may not return our bowels to a healthy state even if the bacteria are able to grow and fill in the void.
The idea behind probiotics is to take so called "good" bacteria and consume them in such a way as to populate the bowel with them creating a healthier state. There are a number of flaws in this theory based on our current state of knowledge though.
1) We don't know which bacteria are "good" - Some bacteria may be good in certain places and not others or when present in combination with certain bacteria but not others. Remember too that we all have very unique microbiomes and it may turn out that a bacteria which is beneficial in one person may have no effect or even be harmful in someone else.
2) We don't know if we can effectively seed the body with new bacteria - It might seem logical that taking a pill filled with a particular bacteria would allow it to grow inside your bowel like seeding your front lawn but that may not work. The desirable bacteria may be absent because the conditions required for them to grow don't exist in the particular body we are trying to put them in. If you spread seed on a bare dry hard patch of your yard it may remain bare for the same reason it was that way in the first place, not enough water, too little sun or some other condition that wasn't conducive to growth. The same may be true when we try to seed an inhospitable bowel with new bacteria.
3) The microbiome is much more complicated then we thought - A defective microbiome may be missing a lot more than one or two species of bacteria. Trying to seed your bowel with "good" bacteria after they have been presumably wiped out may be like trying to repopulate the rain forest after its been stripped bare by seeding it with a few parrots and rubber trees. You may have a some trees and birds but you wont have a rain forest. Putting probiotics into our guts after our diets or medications have altered the normal collection of species may not return our bowels to a healthy state even if the bacteria are able to grow and fill in the void.
What should you do?
A great deal of research is going on in this field but we have only scratched the surface and there is a lot we still don't know. Until we know more it's probably best not to intentionally alter the normal bacteria that inhabit our bodies any more than necessary unless we have good evidence that the benefits will outweigh the possible harm.
Whenever possible limit antibiotic use to those situations that truly require them and for the shortest amount of time needed to clear the infection. All colds and most cases of bronchitis, sore throats, and sinus infection do not require antibiotics and will usually get better just as quickly with rest and over the counter medications that can relieve symptoms until the illness passes on its own.
Probiotics may have some role in treating diseases related to a disturbed microbiome in the future but current preparations have shown no benefit in many studies and mixed results in others. Most claims made by marketers of probiotics are exaggerated and not based on sound science. Attempts to alter the bacterial species in our bodies with probiotics should be done only under the direction of a physician in the limited situations where this has been proven to be helpful.
Whenever possible limit antibiotic use to those situations that truly require them and for the shortest amount of time needed to clear the infection. All colds and most cases of bronchitis, sore throats, and sinus infection do not require antibiotics and will usually get better just as quickly with rest and over the counter medications that can relieve symptoms until the illness passes on its own.
Probiotics may have some role in treating diseases related to a disturbed microbiome in the future but current preparations have shown no benefit in many studies and mixed results in others. Most claims made by marketers of probiotics are exaggerated and not based on sound science. Attempts to alter the bacterial species in our bodies with probiotics should be done only under the direction of a physician in the limited situations where this has been proven to be helpful.
References:
- Infant immune systems set on low to encourage microbiome growth Keeping the immune system in check helps the development of healthy gut bacteria.
- “THE E. COLI MADE ME DO IT”, BY JAMES T. ROSENBAUM, The New Yorker November,2013
- Can We Eat Our Way To A Healthier Microbiome? It's Complicated by MAANVI SINGH NPR, November 08, 2013
- How the gut's "microbiome" affects weight gain, By RYAN JASLOW / CBS NEWS/ October 15, 2013
- Exploring The Invisible Universe That Lives On Us — And In Us by ROB STEIN November 04, 2013
Recent
Are You Really Allergic to Penicillin? The Truth Might Surprise You
January 19th, 2025
Understanding Homeopathy: A Critical Look
October 25th, 2024
HPV Vaccines - Fact and Fiction
July 5th, 2024
Ear Pressure Problems: Navigating Eustachian Tube Dysfunction
June 24th, 2024
Carotid Doppler/Ultrasound Tests: Who should have this test done?
June 19th, 2024
Archive
2024
May
Ozempic - Obesity cure or panacea?GMO's (Genetically Modified Organisms) - Are they truly "Frankenfoods" or our best hope for feeding a hungry world?The Drip Dilemma: Why Healthy People Should Steer Clear of IV TherapyLung Cancer Screening - Is it time to get a CT scan?The Whole Truth Behind Whole Body MRI Scans – Overhyped, Overpriced, and Overrated!Understanding Sinus Infections: Beyond the Common ColdAbdominal Aortic Aneurysms: What You Need to Know
June
2014
March
May
2013
July
August
October
November
Omega 3's (Fish Oil and Flax Seed Oil) who should take them?How do you save a life ? - Just swab your cheekNew Cholesterol Guidelines - What's changed and what does it mean for you?Antibiotics and Probiotics- Why you shouldn't take either without a good reasonPreventing Heart Disease with almonds- Is this study Nuts?