The PSA test - Should you be screened for prostate cancer on your next physical?

PSA
Prostate Specific Antigen Screening Test
PSA ( Prostate Specific Antigen) is a blood test doctors have used to screen for prostate cancer for the past 25 years. Recently the PSA has been in the news because of questions about how useful the test is at reducing deaths from prostate cancer. In this article I will go over the risks and benefits of the test and discuss the current recommendations.
PSA is a protein that is produced in healthy prostate tissue. Prostate cancer cells also make PSA but on average they make more than healthy tissue does. For this reason it was thought that measuring PSA might be a reasonable way to screen for prostate cancer. If the level was higher than average then perhaps cancer was present. Using this reasoning the PSA test was developed and quickly became part of the routine blood work done on men when they had their physical exams.
PSA is a protein that is produced in healthy prostate tissue. Prostate cancer cells also make PSA but on average they make more than healthy tissue does. For this reason it was thought that measuring PSA might be a reasonable way to screen for prostate cancer. If the level was higher than average then perhaps cancer was present. Using this reasoning the PSA test was developed and quickly became part of the routine blood work done on men when they had their physical exams.
While PSA testing became routine, until recently there were no studies that examined the outcome of men who had PSA's done. Yes we were detecting more prostate cancers and probably detecting them earlier but we had no evidence that it actually reduced death rates which is the only thing that really mattered. This is the reason for the current controversy. Two recently published studies have now provided evidence that there may be no survival advantage for men who have PSA's done regularly. As surprising as that seems there was some reason to expect these results.
One of the main issues with the PSA is the problem of false positives and false negatives. This isn't just a problem with the PSA. False positives ( a positive result in someone who does not have the disease) and false negatives ( a negative result in a person who does have the disease) are an unavoidable issue with nearly all tests. It has nothing to do with quality of the lab or the ability of the person performing the test. It is the nature of the tests itself. As stated above, even normal prostate tissue makes PSA but not everyone's prostate makes the same amount of PSA. Similarly not all prostate cancers produce high levels of PSA. If we were to measure the amount of PSA produced by a thousand healthy prostates in men 50-80 yrs old we would find a range from about 0-17 in 90% of men. If we measured the PSA in a thousand men with prostate cancer in the same age group we would find that 90% would have a PSA somewhere between 1 -613.
One of the main issues with the PSA is the problem of false positives and false negatives. This isn't just a problem with the PSA. False positives ( a positive result in someone who does not have the disease) and false negatives ( a negative result in a person who does have the disease) are an unavoidable issue with nearly all tests. It has nothing to do with quality of the lab or the ability of the person performing the test. It is the nature of the tests itself. As stated above, even normal prostate tissue makes PSA but not everyone's prostate makes the same amount of PSA. Similarly not all prostate cancers produce high levels of PSA. If we were to measure the amount of PSA produced by a thousand healthy prostates in men 50-80 yrs old we would find a range from about 0-17 in 90% of men. If we measured the PSA in a thousand men with prostate cancer in the same age group we would find that 90% would have a PSA somewhere between 1 -613.
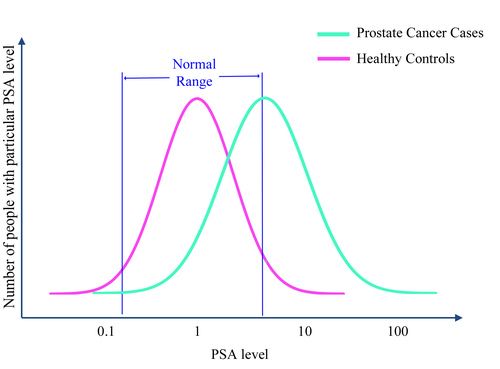
While the prostate cancer patients clearly have a higher PSA on average, we can see that there is a lot of overlap between the two groups. A PSA of 3.0 would be considered a "normal" test result but many patients with prostate cancer might have a PSA of 3.0 or less. Conversely a PSA above 4.0 would be considered elevated but as the graph above shows, there are a significant number of men with normal prostates who will have a PSA in that range.
False negatives can result in a missed diagnosis which is problematic if early detection has been proven to be beneficial. False positives are also a problem because they lead to more invasive and riskier tests such as biopsies. On occasion false positives may also result in unnecessary treatments which exposes the patient to additional risk.
False positive and negative test results are not the only problem with PSA testing though. Most people probably assume that any test which detects cancer earlier could only be a good thing. If there is an effective treatment that improves a patient's outcome when started early, then early detection should save lives. That is not always the case with cancer though. Contrary to popular belief early detection is not always helpful, in part because not all cancers are the same. Some cancers are harmless or nearly so. In those cases early detection won't improve the outcome because treatment is not necessary. Early detection may actually result in a worse outcome if unnecessary treatments are started which result in side effects or complications. Some prostate cancers fit into this category. Among men who live to age 80 ninety percent will develop prostate cancer. Most of them will die of old age though rather than their cancer.
On the other hand some cancers may be so aggressive that no treatment will help. Despite the large number of low grade prostate cancers, prostate cancer as a whole is still the second leading cause of cancer deaths in men. For men with very aggressive prostate cancer early detection may also offer no benefit and may be harmful.
There probably are some men who have a form of prostate cancer which can be treated effectively with early detection, but the question we need to answer is whether those cases balance the cases where men are treated unnecessarily and suffer side effects or even die from the treatment. This is the source of the current controversy.
False negatives can result in a missed diagnosis which is problematic if early detection has been proven to be beneficial. False positives are also a problem because they lead to more invasive and riskier tests such as biopsies. On occasion false positives may also result in unnecessary treatments which exposes the patient to additional risk.
False positive and negative test results are not the only problem with PSA testing though. Most people probably assume that any test which detects cancer earlier could only be a good thing. If there is an effective treatment that improves a patient's outcome when started early, then early detection should save lives. That is not always the case with cancer though. Contrary to popular belief early detection is not always helpful, in part because not all cancers are the same. Some cancers are harmless or nearly so. In those cases early detection won't improve the outcome because treatment is not necessary. Early detection may actually result in a worse outcome if unnecessary treatments are started which result in side effects or complications. Some prostate cancers fit into this category. Among men who live to age 80 ninety percent will develop prostate cancer. Most of them will die of old age though rather than their cancer.
On the other hand some cancers may be so aggressive that no treatment will help. Despite the large number of low grade prostate cancers, prostate cancer as a whole is still the second leading cause of cancer deaths in men. For men with very aggressive prostate cancer early detection may also offer no benefit and may be harmful.
There probably are some men who have a form of prostate cancer which can be treated effectively with early detection, but the question we need to answer is whether those cases balance the cases where men are treated unnecessarily and suffer side effects or even die from the treatment. This is the source of the current controversy.
Until recently there was insufficient evidence to draw a conclusion on the benefits and risks of PSA testing. Most physicians practiced under the assumption that early detection was likely to be beneficial and therefor they routinely ordered PSA tests on men between 40 and 75. What changed were recent studies done in the U.S. (PLCO trial) and Europe ( ERSPC study) and the subsequent recommendation by the U.S. Preventive Services Task Force (USPSTF). The USPSTF is an independent panel of physicians who are experts in primary care and preventive medicine. It is funded by the Department of Health and Human Services with the task of evaluating screening methods based on the best evidence available. Based on the PLCO and ERSPC studies as well as previous evidence the USPSTF came to the conclusion that the benefits of PSA screening did not outweigh the risks. The USPSTF uses a grading system for screening tests and gave the PSA test a grade of D which means "The USPSTF recommends against the service. There is moderate or high certainty that the service has no net benefit or that the harms outweigh the benefits." It is generally recommended that physicians not use screening tests that have a D rating.
There are still some unanswered questions. We do not know whether PSA might still be useful in certain groups that are at higher risk for prostate cancer such as black men and men with a history of prostate cancer among first degree relatives ( father or brother). More studies need to be done to determine if these groups might benefit from PSA screening.
It is a good idea for all patients to discuss their individual situation with their personal physician before deciding whether to have a PSA test, but it appears that for the vast majority of men its best to refrain from using this test.
There are still some unanswered questions. We do not know whether PSA might still be useful in certain groups that are at higher risk for prostate cancer such as black men and men with a history of prostate cancer among first degree relatives ( father or brother). More studies need to be done to determine if these groups might benefit from PSA screening.
It is a good idea for all patients to discuss their individual situation with their personal physician before deciding whether to have a PSA test, but it appears that for the vast majority of men its best to refrain from using this test.
References:
U.S. Preventive Services Task Force: PSA Recommendation Statement
Mortality Results from a Randomized Prostate-Cancer Screening Trial- PLCO trial
Results and participation factors to the European randomized study of screening for prostate cancer (ERSPC) with prostate specific antigen: French departments of Tarn Herault. Prog Urol2009;19:487-98.
Randomised prostate cancer screening trial: 20 year follow-up
Population based age-specific reference ranges for PSA. D. J. Connolly, A. Black, L. J. Murray, A. Gavin, P. F. Keane. 2007 Prostate Cancer Symposium.
Mortality Results from a Randomized Prostate-Cancer Screening Trial- PLCO trial
Results and participation factors to the European randomized study of screening for prostate cancer (ERSPC) with prostate specific antigen: French departments of Tarn Herault. Prog Urol2009;19:487-98.
Randomised prostate cancer screening trial: 20 year follow-up
Population based age-specific reference ranges for PSA. D. J. Connolly, A. Black, L. J. Murray, A. Gavin, P. F. Keane. 2007 Prostate Cancer Symposium.
Recent
Are You Really Allergic to Penicillin? The Truth Might Surprise You
January 19th, 2025
Understanding Homeopathy: A Critical Look
October 25th, 2024
HPV Vaccines - Fact and Fiction
July 5th, 2024
Ear Pressure Problems: Navigating Eustachian Tube Dysfunction
June 24th, 2024
Carotid Doppler/Ultrasound Tests: Who should have this test done?
June 19th, 2024
Archive
2024
May
Ozempic - Obesity cure or panacea?GMO's (Genetically Modified Organisms) - Are they truly "Frankenfoods" or our best hope for feeding a hungry world?The Drip Dilemma: Why Healthy People Should Steer Clear of IV TherapyLung Cancer Screening - Is it time to get a CT scan?The Whole Truth Behind Whole Body MRI Scans – Overhyped, Overpriced, and Overrated!Understanding Sinus Infections: Beyond the Common ColdAbdominal Aortic Aneurysms: What You Need to Know
June
2014
March
May
2013
July
August
October
November
Omega 3's (Fish Oil and Flax Seed Oil) who should take them?How do you save a life ? - Just swab your cheekNew Cholesterol Guidelines - What's changed and what does it mean for you?Antibiotics and Probiotics- Why you shouldn't take either without a good reasonPreventing Heart Disease with almonds- Is this study Nuts?