
OVER AND UNDER ACTIVE THYROID DISORDERS
Thyroid disorders, such as hypothyroidism and hyperthyroidism are very common and they can significantly impact bodily functions, particularly energy regulation. The thyroid, a small gland located in the neck, is one factor governing metabolic processes crucial for maintaining healthy functioning of our other organs. Hypothyroidism refers to an underactive thyroid. if significant enough this can lead to weight gain, dry brittle hair, constipation and fatigue. Conversely, hyperthyroidism signals an overactive thyroid and if it is overactive enough it can lead to symptoms like a rapid, irregular heart rhythm, bone loss and weigh loss.
100 years ago when there were limited ways to diagnose thyroid disorders before symptoms developed it was common to see patients with classic symptoms of an over or underactive thyroid. Today we have very sensitive blood test that can detect thyroid disease long before the point where it causes symptoms. For this reason most patients who are diagnosed with thyroid disease do not have any of the classic symptoms. This allows us to diagnose thyroid disorders and treat them if necessary long before they cause any harm.
100 years ago when there were limited ways to diagnose thyroid disorders before symptoms developed it was common to see patients with classic symptoms of an over or underactive thyroid. Today we have very sensitive blood test that can detect thyroid disease long before the point where it causes symptoms. For this reason most patients who are diagnosed with thyroid disease do not have any of the classic symptoms. This allows us to diagnose thyroid disorders and treat them if necessary long before they cause any harm.
How do we detect thyroid disease?
WHAT DO THE TEST RESULTS MEAN ?
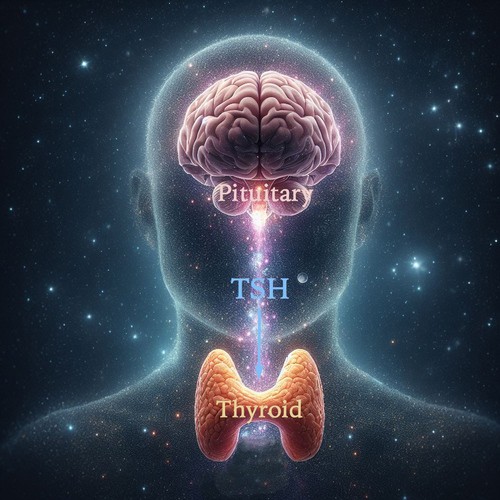
Thyroid disease can be detected with a common set of blood tests collectively called thyroid function tests. These include tests for the hormones made by the thyroid gland (T4 and T3) and an especially important hormone made by the pituitary gland called Thyroid Stimulating Hormone (TSH) which does exactly what it says, It stimulates the thyroid gland.
The pituitary gland sits in the skull just under the brain. It is sort of the master gland. It monitors other glands. If the are producing more of their particular hormone than the body needs it reduces the amount of stimulation it sends to that gland. If they are not producing enough then it increases the stimulation to that gland. In the case of the thyroid gland, if it's not making enough T4 and T3 then the pituitary gland sends out more TSH. If its producing too much thyroid hormone then the pituitary reduces the amount of TSH.
Because the pituitary is the best judge of whether our thyroid hormone levels are meeting our needs the TSH is the most sensitive test we have to detect thyroid disorders. It is a more accurate indicator than measurements of the T4 or T3 thyroid hormones. Therefor this is the first test your doctor will usually do to screen for thyroid disease. If this test is normal then there is no reason to waste money and resources doing the other tests.
The pituitary gland sits in the skull just under the brain. It is sort of the master gland. It monitors other glands. If the are producing more of their particular hormone than the body needs it reduces the amount of stimulation it sends to that gland. If they are not producing enough then it increases the stimulation to that gland. In the case of the thyroid gland, if it's not making enough T4 and T3 then the pituitary gland sends out more TSH. If its producing too much thyroid hormone then the pituitary reduces the amount of TSH.
Because the pituitary is the best judge of whether our thyroid hormone levels are meeting our needs the TSH is the most sensitive test we have to detect thyroid disorders. It is a more accurate indicator than measurements of the T4 or T3 thyroid hormones. Therefor this is the first test your doctor will usually do to screen for thyroid disease. If this test is normal then there is no reason to waste money and resources doing the other tests.
A high TSH means the pituitary gland thought that the body was not getting enough thyroid hormone to meet its needs. and a low TSH means just the opposite. This can be a bit confusing sometimes for patients because a High TSH means there may be an Underactive thyroid and a Low TSH means there may be an Overactive thyroid which is opposite of what someone might think at first.
Causes and treatment of Thyroid Disorders
There are many possible causes of thyroid disorders and the things that cause hyperthyroidism are different than the things that cause hypothyroidism although there is some overlap. Because these are very different conditions the treatments are also different as I will outline below.
It's important to understand that a high or low TSH level does not necessarily mean that treatment is required. Remember this just means that the pituitary is doing a little more or less work than it usually does to get the thyroid to produce the necessary amount of thyroid hormone but if that level of stimulation provides the correct amount of T3 and T4 to meet the body's needs than no treatment is needed. The decision to provide treatment isn't always determined by the TSH level alone. Often the TSH, the T3 and T4, and symptoms are used in combination to make the decision about treatment.
It's important to understand that a high or low TSH level does not necessarily mean that treatment is required. Remember this just means that the pituitary is doing a little more or less work than it usually does to get the thyroid to produce the necessary amount of thyroid hormone but if that level of stimulation provides the correct amount of T3 and T4 to meet the body's needs than no treatment is needed. The decision to provide treatment isn't always determined by the TSH level alone. Often the TSH, the T3 and T4, and symptoms are used in combination to make the decision about treatment.

Hypothyroidism
HYPOTHYROIDISM - The underactive thyroid - Usually with a High TSH
CAUSES: There are many possible causes of hypothyroidism although the vast majority of cases are caused by the first item on the list below known as Autoimmune Thyroiditis or Hashimoto's Thyroiditis. This condition is 3-4 times more common in women than men and often there is a strong genetic component to it.
Hashimoto's Thyroiditis (Autoimmune Thyroiditis) is the most common cause of hypothyroidism in developed countries. It occurs when the body's immune system mistakenly attacks the thyroid gland, leading to inflammation and eventual damage, impairing its ability to produce hormones.
Other less common causes:
Hashimoto's Thyroiditis (Autoimmune Thyroiditis) is the most common cause of hypothyroidism in developed countries. It occurs when the body's immune system mistakenly attacks the thyroid gland, leading to inflammation and eventual damage, impairing its ability to produce hormones.
Other less common causes:
- Iodine Deficiency: Iodine is essential for the production of thyroid hormones. In regions where iodine intake is low, such as certain parts of the world with soil deficient in iodine, hypothyroidism can develop due to insufficient iodine intake.
- Thyroid Surgery or Radioactive Iodine Treatment: Thyroidectomy (surgical removal of the thyroid gland) or radioactive iodine treatment for hyperthyroidism can lead to hypothyroidism, as these procedures can damage or remove the thyroid gland.
- Medications: Certain medications, such as lithium (used to treat bipolar disorder), amiodarone (used to treat heart arrhythmias), and some cancer treatments, can interfere with thyroid hormone production and lead to hypothyroidism.
- Congenital Hypothyroidism: Some infants are born with an underdeveloped or absent thyroid gland (congenital hypothyroidism), or they may have a thyroid gland that doesn't function properly. This can lead to inadequate thyroid hormone production from birth if not detected and treated promptly.
- Pituitary or Hypothalamic Disorders: Hypothyroidism can result from disorders affecting the pituitary gland or hypothalamus, which are parts of the brain that regulate thyroid hormone production. If these glands fail to produce enough thyroid-stimulating hormone (TSH) or thyrotropin-releasing hormone (TRH), the thyroid gland won't receive the signal to produce hormones adequately.
- Thyroiditis: Inflammation of the thyroid gland, which can occur due to various reasons such as viral infections or postpartum thyroiditis, can lead to temporary or permanent hypothyroidism depending on the severity and cause of inflammation.
- Certain Medical Conditions: Some medical conditions, such as Turner syndrome, Down syndrome, or autoimmune diseases like rheumatoid arthritis or lupus, are associated with a higher risk of developing hypothyroidism.
TREATMENT: Treatment for hypothyroidism involves replacing inadequate levels of thyroid hormone with a synthesized version of the T4 hormone called Levothyroxine, sometimes known by its brand name Synthroid. This hormone is available in pill form and, once absorbed, is converted into the active hormone T3. Occasionally, products containing both T4 and T3 in the pill are used, but this is rarely necessary.
Although the normal range for TSH is usually between 0.25 and 4.5 at most labs treatment is not usually recommended unless the TSH is 10 or higher or the TSH is between 4.6 and 9.9 and the patient has significant symptoms. Symptoms are things like fatigue, constipation, dry skin, and weight gain but all of these symptoms are extremely common and rarely ever due to thyroid disease so what we are looking for are symptoms that are well beyond the normal symptoms that many people have.
Once treatment is decided upon and initiated its necessary to bring the patient back to repeat the TSH. Usually, we wait about 6 weeks to do this because it takes that long for the pituitary-thyroid system to settle out at a stable level once the medication is started. If the repeat TSH is not in the desired range and the dose of the medication needs to be adjusted, we again wait 6 weeks to recheck the bloodwork. The goal is to bring the TSH down to the lower half of the normal range ideally between around 1 and 2.5. Once this is achieved the level is usually checked about every six months from that point on. Patients who have hypothyroidism will usually have this condition for life. It does not usually correct because the damaged thyroid tissue cannot be restored, so lifetime treatment is required in most cases.
Side effects of thyroid medication are usually minimal. Remember all we are doing is providing the body with the same hormone it makes on its own but can no longer make enough of. Any side effects would occur only if the dose was too high or too low and would mimic an overactive or underactive thyroid. For this reason, it's important to make sure the levels are checked twice a year.
Although the normal range for TSH is usually between 0.25 and 4.5 at most labs treatment is not usually recommended unless the TSH is 10 or higher or the TSH is between 4.6 and 9.9 and the patient has significant symptoms. Symptoms are things like fatigue, constipation, dry skin, and weight gain but all of these symptoms are extremely common and rarely ever due to thyroid disease so what we are looking for are symptoms that are well beyond the normal symptoms that many people have.
Once treatment is decided upon and initiated its necessary to bring the patient back to repeat the TSH. Usually, we wait about 6 weeks to do this because it takes that long for the pituitary-thyroid system to settle out at a stable level once the medication is started. If the repeat TSH is not in the desired range and the dose of the medication needs to be adjusted, we again wait 6 weeks to recheck the bloodwork. The goal is to bring the TSH down to the lower half of the normal range ideally between around 1 and 2.5. Once this is achieved the level is usually checked about every six months from that point on. Patients who have hypothyroidism will usually have this condition for life. It does not usually correct because the damaged thyroid tissue cannot be restored, so lifetime treatment is required in most cases.
Side effects of thyroid medication are usually minimal. Remember all we are doing is providing the body with the same hormone it makes on its own but can no longer make enough of. Any side effects would occur only if the dose was too high or too low and would mimic an overactive or underactive thyroid. For this reason, it's important to make sure the levels are checked twice a year.

Hyperthyroidism
HYPERTHYROIDISM - The overactive thyroid - Usually with a Low TSH
CAUSES: As with hypothyroidism there are a number of things that can cause hyperthyroidism. Of these by far Graves' disease is the cause in the vast majority of cases.
Graves' Disease is an autoimmune disorder is the most common cause of hyperthyroidism. It leads to the overproduction of thyroid hormone due to antibodies stimulating the thyroid gland.
Other less common causes
Graves' Disease is an autoimmune disorder is the most common cause of hyperthyroidism. It leads to the overproduction of thyroid hormone due to antibodies stimulating the thyroid gland.
Other less common causes
- Toxic Multinodular Goiter (Plummer's Disease): This condition involves the formation of multiple nodules in the thyroid gland, which produce thyroid hormones independently of the body's regulatory mechanisms, leading to excessive hormone production.
- Thyroiditis: Inflammation of the thyroid gland, whether due to viral infections, autoimmune diseases, or other causes, can cause temporary hyperthyroidism as thyroid hormone stored in the gland is released into the bloodstream.
- Excessive Iodine Intake: Consuming high levels of iodine through diet, medications, or supplements can lead to hyperthyroidism, especially in individuals with underlying thyroid conditions.
- Thyroid Nodules: Certain types of thyroid nodules, such as toxic adenomas, can autonomously produce thyroid hormone, leading to hyperthyroidism.
- Excessive Thyroid Hormone Replacement Therapy: Overmedication with thyroid hormone replacement medications (e.g., levothyroxine) can lead to hyperthyroidism.
- Tumors of the Thyroid or Pituitary Gland: Benign or malignant tumors of the thyroid gland or pituitary gland can disrupt normal thyroid hormone regulation, leading to excessive hormone production.
- Excess Thyroid-Stimulating Hormone (TSH): Rarely, tumors of the pituitary gland (pituitary adenomas) can produce excessive TSH, which stimulates the thyroid gland to produce too much thyroid hormone.
- Subacute Thyroiditis: This condition involves inflammation of the thyroid gland, often following a viral infection, which can initially cause hyperthyroidism due to the release of stored thyroid hormone, followed by temporary hypothyroidism as the gland recovers.
- Overconsumption of Thyroid Hormone Supplements: Ingesting excessive amounts of thyroid hormone supplements, often in attempts at weight loss or performance enhancement, can lead to hyperthyroidism.
TREATMENT: The treatment for hyperthyroidism is different that the treatment for hypothyroidism but the goal it the same, to provide the necessary amount of thyroid hormones to the body to meet its needs. Treatment for hyperthyroidism aims to reduce the production of thyroid hormone, normalize thyroid function, and alleviate symptoms. Here are common treatment options:
The choice of treatment depends on various factors, including the underlying cause of hyperthyroidism, the severity of symptoms, the presence of comorbidities, and patient preference. It's essential for individuals with hyperthyroidism to work closely with their healthcare team to determine the most appropriate treatment plan for their specific situation. Because of the complexity of the treatment, hyperthyroidism is usually treated by an endocrinologist since they are the specialists who are experts in hormone disorders.
- Antithyroid Medications: These medications, such as methimazole (Tapazole) or propylthiouracil (PTU), work by inhibiting the thyroid gland's ability to produce thyroid hormone. They are often used as the first-line treatment for hyperthyroidism, especially in Graves' disease or thyroiditis.
- Radioactive Iodine Therapy (RAI): This treatment involves ingesting a radioactive form of iodine, which selectively destroys the thyroid tissue, thereby reducing hormone production. RAI is commonly used as a definitive treatment for hyperthyroidism, particularly in Graves' disease, and often leads to hypothyroidism as a long-term consequence, requiring lifelong thyroid hormone replacement therapy.
- Thyroidectomy: Surgical removal of part or all of the thyroid gland (subtotal or total thyroidectomy) may be recommended in cases where antithyroid medications are ineffective or not tolerated, or if RAI is contraindicated. Thyroidectomy is usually reserved for specific situations, such as large goiters, thyroid nodules, or when cancer is suspected.
- Beta-Blockers: Medications like propranolol or atenolol may be prescribed to alleviate symptoms such as rapid heart rate, tremors, and anxiety associated with hyperthyroidism. Beta-blockers do not treat the underlying thyroid condition but can provide symptomatic relief while other treatments take effect.
- Symptomatic Treatment: In addition to specific treatments targeting the thyroid gland, healthcare providers may prescribe medications to manage symptoms associated with hyperthyroidism, such as anti-anxiety medications for nervousness or sleep disturbances, or eye drops for eye symptoms in Graves' ophthalmopathy.
- Regular Monitoring: Regardless of the chosen treatment modality, regular monitoring of thyroid function is essential to assess treatment effectiveness, adjust medication dosages if necessary, and monitor for potential complications or side effects.
The choice of treatment depends on various factors, including the underlying cause of hyperthyroidism, the severity of symptoms, the presence of comorbidities, and patient preference. It's essential for individuals with hyperthyroidism to work closely with their healthcare team to determine the most appropriate treatment plan for their specific situation. Because of the complexity of the treatment, hyperthyroidism is usually treated by an endocrinologist since they are the specialists who are experts in hormone disorders.