Definition and Diagnosis
Our bodies are constantly resorbing old bone and building new bone to keep our bones healthy. When this process results in more bone resorption than formation bones can become weak and are more likely to fracture. We call this condition osteoporosis.
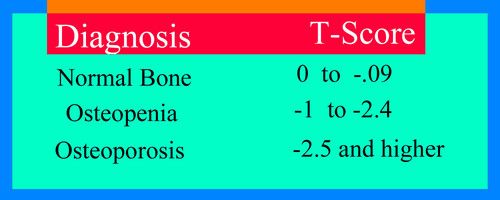
Osteoporosis is diagnosed with the use of a Bone Density Test. The test gives us something called a T-Score. The more negative the T-score the weaker the bones. A normal T-Score is 0 to -0.9. If the number is from -1 to -2.4 we call this osteopenia which means the bones have become weaker but the risk of a fracture has not reached critical levels yet. Osteoporosis is defined as a T-score greater than or equal to -2.5. At this level there is a significant increased risk of fracture.
Risk Factors
Some people live to a ripe old age and never get osteoporosis while others show evidence of the disease in their 40's. There are many factors that determine who gets osteoporosis and when. Some of these factors are under our control and others are not.
- Age – risk goes up with age
- Sex – women are at greater risk than men
- Caucasian or Asian race are at increased risk
- Family history – people who have a parent or sibing with a history of hip fracture are at increased risk
- Frame size – people who are small framed are at higher risk
- Steroid use – frequent use of steroids increases risk
- Sedentary lifestyle
- Smoking
- Alcohol use – more than two drinks per day increases risk.
Who needs to be screened?
Although men can develop osteoporosis this is relatively uncommon unless they have unusual risk factors. All women over 65 should be screened for osteoporosis and women with multiple risk factors as outlined above should begin screening no later than age 60.
How often should bone density tests be repeated?
While there is no consensus agreement on how often to repeat bone density tests one recommendation suggests repeat bone density testing every couple of years in patients receiving treatment for osteoporosis. In addition it has been suggested that patients with osteopenia might repeat their bone density test depending on their results according to the following schedule.
FIRST BONE DENSITY
AVERAGE RISK - AGE 65
HIGH RISK - AGE 60
REPEAT BONE DENSITY
FREQUENCY OF REPEAT BONE DENSITY TESTS DEPENDS ON THE RESULTS OF FIRST TEST.
AVERAGE RISK - AGE 65
HIGH RISK - AGE 60
REPEAT BONE DENSITY
FREQUENCY OF REPEAT BONE DENSITY TESTS DEPENDS ON THE RESULTS OF FIRST TEST.
- IF FIRST BONE DENSITY RESULT IS -1.0 TO -1.49, REPEAT EVERY 10-15 YEARS
- -1.5 TO -1.99 REPEAT EVERY 3-5 YEARS
- -2.0 TO -2.49, REPEAT EVERY 2 YEARS
Treatment Options
Treatment depends on the diagnosis.
Osteopenia - In general, patients who only have osteopenia do not need to take prescription medication. The recommended treatment for this condition is Calcium, Vitamin D, Weight Bearing exercises and if they smoke they should quit.
Osteoporosis - Patients with osteoporosis have already suffered significant bone loss. Non-medication treatments may slow further bone loss but will not rebuild bone that has already been lost. For this reason most patients with osteoporosis should also be offered treatment with one of the medications ilsted below.
Osteopenia - In general, patients who only have osteopenia do not need to take prescription medication. The recommended treatment for this condition is Calcium, Vitamin D, Weight Bearing exercises and if they smoke they should quit.
Osteoporosis - Patients with osteoporosis have already suffered significant bone loss. Non-medication treatments may slow further bone loss but will not rebuild bone that has already been lost. For this reason most patients with osteoporosis should also be offered treatment with one of the medications ilsted below.
Non-Medication Treatments

- Calcium
- Vitamin D
- Vitamin K
- Weight bearing exercises
- Quitting Smoking
Non-medication treatments for osteoporosis focus on lifestyle modifications and various interventions aimed at preventing bone loss and reducing the risk of fractures. Here are some common non-medication treatments along with the strength of evidence supporting them and potential side effects:
Vitamins and calcium are actually medications with both effects and side effects like any medication but since they are commonly listed with non-medication options they will be listed here for consistency.
It's crucial to note that the effectiveness of these non-medication treatments may vary depending on individual factors such as age, overall health, and the severity of osteoporosis. Consulting with a healthcare professional is recommended to develop a personalized treatment plan tailored to individual needs and circumstances.
It's important to keep in. mind that while every drug has some listed side effects, even the common ones only occur in a small portion of patients. You can read more about medication side effects at the bottom of the page.
Vitamins and calcium are actually medications with both effects and side effects like any medication but since they are commonly listed with non-medication options they will be listed here for consistency.
- Calcium:
- Strength of Evidence: Evidence is lacking to support the use of calcium supplementation to support bone health,
- Potential Side Effects: Excessive calcium intake may lead to constipation, kidney stones, and impaired absorption of other minerals like iron and zinc. It's essential to avoid excessive doses, and it's often recommended to obtain calcium from dietary sources when possible.
- Vitamin D:
- Strength of Evidence: Evidence is lacking to support the use of Vitamin D in the prevention of or treatment of osteoporosis
- Potential Side Effects: Vitamin D toxicity is rare but can occur with very high doses. Symptoms may include nausea, vomiting, weakness, and kidney problems. It's essential to monitor vitamin D levels and follow dosing recommendations.
- Vitamin K:
- Strength of Evidence: Scientific evidence, including meta-analyses and clinical trials, suggests that vitamin K supplementation or increased dietary intake may help reduce the risk of osteoporosis and fractures by improving bone mineral density and bone quality. However, further research, including long-term studies, is warranted to confirm these findings and determine the optimal dosage and duration of vitamin K supplementation for bone health benefits.
- Potential Side Effects: Vitamin K can interact with some medications such as Warfarin. High doses may interfere with Vitamin E absorption and can sometimes cause gastrointestinal symptoms
- Exercise:
- Strength of Evidence: There is moderate evidence to support the benefits of exercise on reduction of osteoporotic fractures. Regular weight-bearing and muscle-strengthening exercises are beneficial for improving bone density, strength, and balance, thereby reducing the risk of fractures.
- Potential Side Effects: Exercise, when done correctly, generally has minimal side effects. However, improper form or excessive intensity may lead to musculoskeletal injuries. It's essential to start gradually and consult a healthcare professional for personalized exercise recommendations.
- Smoking Cessation:
- Strength of Evidence: Smoking is associated with an increased risk of osteoporosis and fractures. Quitting smoking can help slow bone loss and reduce fracture risk.
- Potential Side Effects: Nicotine withdrawal symptoms may occur when quitting smoking, including irritability, anxiety, and cravings. Additionally, some individuals may experience weight gain. However, the long-term benefits of smoking cessation outweigh these potential side effects and there are many options and resources available now to make quitting more successful.
- Healthy Diet:
- Strength of Evidence: A balanced diet rich in nutrients essential for bone health, including calcium, vitamin D, protein, magnesium, and vitamin K, can help support bone density and overall health.
- Potential Side Effects: A healthy diet typically has minimal side effects. However, excessive intake of certain nutrients or dietary supplements may lead to adverse effects. It's essential to maintain balance and moderation in dietary choices.
- Fall Prevention Strategies:
- Strength of Evidence: Implementing fall prevention strategies, such as removing hazards in the home, improving lighting, using assistive devices, and practicing balance exercises, can help reduce the risk of fractures, especially in older adults.
- Potential Side Effects: Fall prevention strategies themselves generally have no direct side effects. However, some individuals may find certain interventions challenging to implement, such as changes to the home environment or adjusting to assistive devices.
It's crucial to note that the effectiveness of these non-medication treatments may vary depending on individual factors such as age, overall health, and the severity of osteoporosis. Consulting with a healthcare professional is recommended to develop a personalized treatment plan tailored to individual needs and circumstances.
It's important to keep in. mind that while every drug has some listed side effects, even the common ones only occur in a small portion of patients. You can read more about medication side effects at the bottom of the page.
Medications

While the non-medication interventions listed above may slow the progression of osteoporosis, they will not reverse the bone loss that has already occurred. By the time a patient has bone loss severe enough to meet the definition of osteoporosis, medications are the only way to significantly reduce the risk of a fracture. The availble options are listed below.
Below is a list of some common medications used to treat osteoporosis, along with descriptions of how they work, their proven benefits, and potential common side effects and risks:
It's important to note that the choice of medication depends on factors such as age, sex, medical history, and preferences, and should be made in consultation with a healthcare provider. Additionally, individual responses to medications can vary, so close monitoring for both efficacy and adverse effects is essential.
- Bisphosphonates:
- Examples: Alendronate (Fosamax), Risedronate (Actonel), Ibandronate (Boniva), Zoledronic acid (Reclast, Zometa)
- How Administered: Oral pill daily, weekly, or monthly except Zoledronic acid which is IV once a year
- How they work: Bisphosphonates inhibit the activity of osteoclasts, the cells responsible for breaking down bone tissue, thereby slowing down bone loss and reducing fracture risk.
- Proven benefits: Increased bone mineral density (BMD) and reduced risk of fractures, particularly in the spine and hip.
- Common side effects and risks: Gastrointestinal issues like heartburn and nausea, esophageal irritation, rare cases of osteonecrosis of the jaw (ONJ), and atypical femoral fractures.
- Selective Estrogen Receptor Modulators (SERMs):
- Examples: Raloxifene (Evista)
- How Administered: Oral pill daily
- How they work: SERMs like raloxifene act similarly to estrogen in some tissues, helping to preserve bone density by reducing bone resorption.
- Proven benefits: Reduced risk of vertebral fractures in postmenopausal women.
- Common side effects and risks: Hot flashes, leg cramps, and increased risk of blood clots.
- Calcitonin:
- Examples: Salmon calcitonin (Miacalcin, Fortical)
- How Administered: Injection daily
- How it works: Calcitonin inhibits osteoclast activity and may also have some pain-relieving effects.
- Proven benefits: Reduction in vertebral fracture risk and some pain relief in patients with osteoporosis.
- Common side effects and risks: Nasal irritation or dryness (for intranasal calcitonin), and flushing or nausea (for injected calcitonin).
- Teriparatide (PTH analog):
- Examples: Teriparatide (Forteo)
- How Administered: Injection daily
- How it works: Teriparatide is a synthetic form of parathyroid hormone (PTH) that stimulates bone formation by osteoblasts, leading to increased bone density.
- Proven benefits: Significant increases in BMD and reduction in fracture risk, especially vertebral fractures.
- Common side effects and risks: Nausea, dizziness, leg cramps, and potential risk of osteosarcoma (bone cancer) in rats, although this risk has not been definitively established in humans.
- Denosumab (RANK ligand inhibitor):
- Examples: Denosumab (Prolia, Xgeva)
- How Administered: Injection once every 6 months
- How it works: Denosumab inhibits the RANK ligand, a protein involved in the formation, function, and survival of osteoclasts, thereby reducing bone resorption.
- Proven benefits: Increased BMD and reduced risk of vertebral, non-vertebral, and hip fractures.
- Common side effects and risks: Skin infections, hypocalcemia (low blood calcium levels), and rare cases of osteonecrosis of the jaw (ONJ).
- Estrogen/Hormone Therapy:
- Examples:
- Conjugated estrogens (Premarin)
- Estrogen and progestin combinations (Prempro, Activella)
- How Administered: Oral pill daily
- How it works: Estrogen helps maintain bone density by inhibiting bone resorption and stimulating bone formation.
- Proven benefits: Reduced risk of fractures, particularly vertebral fractures, in postmenopausal women.
- Common side effects and risks: Increased risk of blood clots, stroke, and breast cancer when used long-term, which has led to a decline in its use for osteoporosis treatment.
- Examples:
- Evenity (Generic: Romosozumab)
- How Administered: Subcutaneous injection administered once monthly.
- How it works: Acts as a monoclonal antibody that inhibits sclerostin, thereby increasing bone formation and decreasing bone resorption, leading to increased bone mineral density.
- Proven Benefits: Demonstrated to significantly reduce the risk of fractures in postmenopausal women with osteoporosis.
- Common Side Effects: Joint pain, headache, pain in the extremities, and hypersensitivity reactions such as rash or itching.
It's important to note that the choice of medication depends on factors such as age, sex, medical history, and preferences, and should be made in consultation with a healthcare provider. Additionally, individual responses to medications can vary, so close monitoring for both efficacy and adverse effects is essential.